The National Breast Cancer Coalition (NBCC) is a grassroots organization dedicated to ending breast cancer through action and advocacy. The following are a few statistics that speak to the need to end this deadly disease.
Download the 2024 Facts & Figures in English and Spanish (PDF).
In 2020 there were 685,000 deaths from breast cancer globally. (WHO, 2021).
In 2024, it is estimated that 42,250 women and 530 men in the United States will die of breast cancer. (Siegel et al., 2024).
Excluding basal cell and squamous cell skin cancers and carcinomas in situ, breast cancer is the most commonly diagnosed cancer among women in the U.S.
In 2024, there will be an estimated 313,510 new cases of invasive breast cancer diagnosed in women; 2790 new cases diagnosed in men, and an additional 56,500 new cases of ductal carcinoma in situ (DCIS) diagnoses in women. (Siegel et al., 2024)
Note: Data available from 2020 were excluded from trend and lifetime risk analyses to account for disruptions in health care related to the COVID-19 pandemic. Also, annual incidence counts of lobular carcinoma in situ are no longer measured following its removal from the 2017 edition of the AJCC breast cancer staging program.
 Lifetime Risk
Lifetime Risk
In the United States, a woman’s lifetime risk of being diagnosed with invasive breast cancer has increased since 1975. (ACS, 2022; Feuer et al., 1993)
2017-2019: 1 in 8 (13%)
1975-1977: 1 in 11 (9.1%)
Incidence By Age
Older women are more likely to get invasive breast cancer than younger women. From 2015-2019, the median age of a breast cancer diagnosis was 62 years of age. (ACS, 2022)
Progress in reducing breast cancer mortality has slowed in recent years, from 2% to 3% annually during the 1990s and 2000s to 1% annually from 2013 to 2021. (ACS, 2022, Siegel et al., 2024)
While the breast cancer mortality rate has declined, the number of women and men who die each year is rising and will continue to rise as the aging population grows.
Mortality By Age
From 2016-2020, the median age at death from breast cancer was 70 years of age. (NCI, 2022)

 RACIAL DISPARITIES
RACIAL DISPARITIESDespite a similar incidence, mortality from breast cancer among Black women is 41% higher compared with White women. (Siegel et al., 2024; ACS, 2022)
The risk of local and distant (metastatic) recurrence varies greatly based on many factors. Estimates of long-term cumulative risk range from about 5% to 60%, with most falling between 10%-30%. Furthermore, recurrence risk remains elevated more than 3 decades from the primary diagnosis. (Saphner et al., 1996; Colleoni et al., 2016; Pan et al., 2017; Pedersen et al., 2022)
As of January 2022, there were an estimated >4 million women living with a history of breast cancer in the U.S.. (Miller et al., 2022)
It is estimated that in 2018, 140,230 women in the U.S. were living with metastatic breast cancer. By 2025, this number is expected to increase to 169,347. (Gallicchio et al., 2022).
Only 5-10% of breast cancers are hereditary. The strongest risks for breast cancer are age and being assigned female at birth.
Other non-modifiable risk factors include: (ACS, 2024; CDC, 2022; CDC, 2022)
Risk factors that are potentially modifiable include:
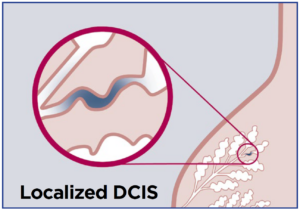 DCIS AND SCREENING
DCIS AND SCREENINGThe diagnosis of ductal carcinoma in situ (DCIS) was rare before 1980, but the widespread adoption of screening mammography led to a massive increase in DCIS diagnosis. From 1980-2000, women aged 20-49 experienced a 400% increase in DCIS diagnoses, and women over the age of 50 experienced over a 900% increase in diagnosis. (NCI, 2000-2019)
Overdiagnosis of breast cancer (i.e., cancer that would never become a problem) by screening mammography is difficult to determine, with most credible estimates ranging from 11%-22%. False positive and false negative mammography results are also possible. Over a 10-year period, more than half of women getting an annual mammogram will receive a false-positive result. (Ryser et al., 2022; Nelson et al., 2016; ACS, 2024, Hubbard et al., 2011).
The current methods of treatment in use in the U.S. are:
NBCC acknowledges that breast cancer impacts people of all gender identities.